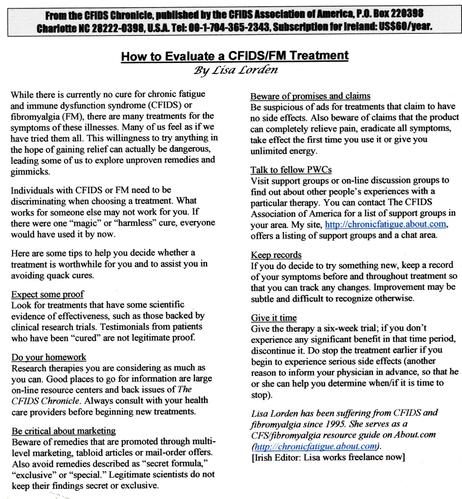
Just clearing out some old files and came across this for around 25 years ago in case of interest to anyone: "How to Evaluate a CFIDS/FM Treatment".
#MyalgicEncephalomyelitis #ChronicFatigueSyndrome #MEcfs #CFS #PwME @mecfs #chronicillness #Fibromyalgia #Fibro #FMS #FM