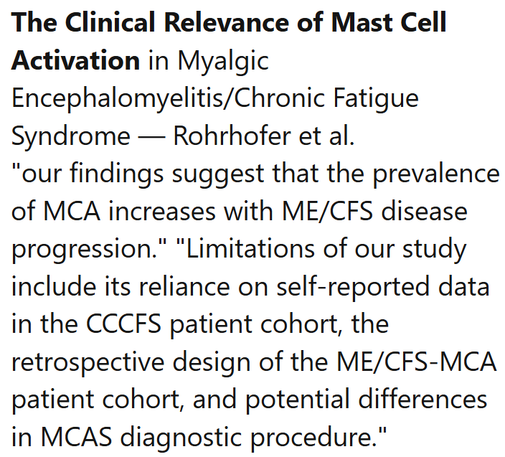
Brayden Yellman, MD | Underappreciated Co-Morbidities in ME/CFS
video uploaded Oct. 16, 2025
https://youtu.be/od0epKW19og
[13:03] hydroxyurea used to treat a person with POTS and MCAS
Here's an article on the topic:
Efficacy and toxicity of hydroxyurea in mast cell activation syndrome patients refractory to standard medical therapy: retrospective case series [2022]
https://pmc.ncbi.nlm.nih.gov/articles/PMC9388361/
"First used 60 years ago for chronic myeloproliferative neoplasms, HU is now standard of care in reducing the severity of sickle cell disease (SCD) (McGann and Ware 2015). In this context, it is of interest that in animal models and human subjects with SCD, medications that reduce MC activation decreased bone pain (Vincent et al. 2013, 2016). HU also inhibits replication of human immunodeficiency virus-1 (HIV-1) and has been used in therapy of cyanotic congenital heart disease (Lori and Lisziewicz 2000; Reiss et al. 2007). A theoretic explanation for effectiveness of HU in these diseases include reducing MC activity independent of anti-proliferative effects. HU could decrease activity and ability of GI mucosal MCs that capture HIV-1 and mediate trans-infection of CD4 + T cells (Jiang et al. 2015). Similarly, HU could reduce the activity of the increased numbers of chymase-containing MCs in lung tissue of congenital heart disease patients and, thereby, decrease severity of these pulmonary and cardiac diseases (Hamada et al. 1999)."
The mechanisms are probably quite complex. One facet is that hydroxyurea increases fetal hemoglobin production and RBC membrane flexibility - which could increase O2 perfusion. Hypoxia activates mast cells.
#MECFS #MCAS #POTS #DrugRepurposing #hydroxyurea #MastCells #immunology