Quick rant on Cigna's absolutely ridiculous policies. Someone arbitrarily decided at some point over the last few months to remove Albuterol from coverage unless the doctor files a "prior use authorization." I literally got my refill through MDLIVE, a company *OWNED BY Cigna*, that was scheduled through the Cigna site. The doctor obviously didn't know a prior use authorization was required (nor was it previously). I now have to waste more time, in addition to paying out of pocket since the next available MDLive appointment in my network is conveniently after I'm likely to be out of my rescue inhaler - you know, breathing medication.
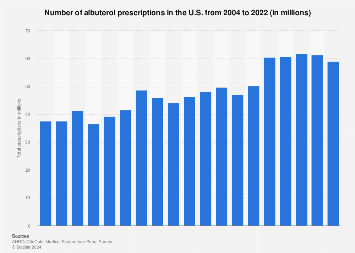
Albuterol is not an uncommon drug. Sure, prescriptions for it are up. But I'll also note that I never needed it until after a respiratory infection that didn't test positive for COVID or RSV. I'll bet a lot of the increases follow that same pattern. I've talked to several people in their 30's and 40's that are on inhalers for the first time in their lives after COVID.
I'll never condone murder in the streets, but I also understand how Luigi got radicalized. And real talk: he saved lives. There shouldn't be profit in healthcare. It's hurting people. I can afford the $35 out of pocket. Many can't. Anyone who profits from denying people the healthcare they pay is human garbage.
https://www.statista.com/statistics/781622/albuterol-prescriptions-number-in-the-us/